-
Publish Your Research/Review Articles in our High Quality Journal for just USD $99*+Taxes( *T&C Apply)
Offer Ends On
Julieth Isacka Koloseni* and Stephen Nyamsaya
Corresponding Author: Julieth Isacka Koloseni, Department of Ophthalmology, Mbeya Zonal Referral Hospital P.O. Box 419, Mbeya, Tanzania.
Received: May 09, 2025 ; Revised: May 16, 2025 ; Accepted: May 19, 2025 ; Available Online: May 21, 2025
Citation: Koloseni JI & Nyamsaya S. (2025) Epidemiology and Risk Factors of Primary Open-Angle Glaucoma: Hospital-Based Evidence and Global Perspectives (2020-2025). J Clin Ophthalmol Optom Res, 3(1): 1-6.
Copyrights: ©2025 Koloseni JI & Nyamsaya S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Views & Citations
Likes & Shares
Background: Primary open-angle glaucoma (POAG) is a major cause of irreversible blindness globally, with a disproportionately higher burden in African populations due to genetic, clinical, and socioeconomic factors. Advances in genetic profiling and systemic risk identification demand updated epidemiological data, especially in resource-limited settings like Tanzania.
Objective: To assess the prevalence, clinical characteristics, and risk factors of POAG by integrating a 2014 hospital-based study from Muhimbili National Hospital with global literature (2020–2025), to guide context-specific screening strategies.
Methodology: This study used a dual approach: a hospital-based cross-sectional analysis and a systematic literature review. Data from 876 new patients diagnosed with POAG at Muhimbili National Hospital in 2014 were analyzed using descriptive statistics and logistic regression. A PRISMA-guided review of twenty-two studies (2020–2025) from PubMed, Embase, and Web of Science provided global context, summarized through narrative synthesis. Ethical approval was secured to protect participant rights.
Result: The hospital study reported a POAG prevalence of 6.6% (95% CI: 5.0-8.5%), exceeding the 4.0% estimated African population rate. Most cases were male (67.2%), aged ≥56 years (70.7%), and bilateral. Elevated intraocular pressure (IOP) (21-26 mmHg) was present in 82.8%, while 79.3% had central corneal thickness <540 μm. Myopia (68.9%), family history (55.2%), and visual field defects were common. High IOP was the strongest risk factor (OR 57.32, 95% CI: 13-252.7, p<0.001). The review confirmed the importance of IOP and thin CCT, and highlighted emerging risk factors such as polygenic risk scores (HR 1.25 per SD), myopia, and hypertension (OR 1.67).
Conclusion: Primary open-angle glaucoma poses a significant burden in African settings. Targeted screening, including IOP checks, genetic profiling, and comorbidity management, is essential. Strengthening community programs and access to diagnostics will aid early detection. Future research should focus on affordable tools and longitudinal studies to promote equitable glaucoma care.
Keywords: Primary open-angle glaucoma, Intraocular pressure, Risk factors, Tanzania, Epidemiology
INTRODUCTION
Primary open-angle glaucoma (POAG) is the most prevalent form of glaucoma globally, characterized by progressive optic nerve damage, retinal ganglion cell loss, and corresponding visual field defects. It is a leading cause of irreversible blindness, affecting an estimated 68.56 million individuals worldwide as of 2020, with the burden expected to rise to 111.8 million by 2040 due to aging populations and increased life expectancy [1,2]. POAG often remains asymptomatic until advanced stages, making early detection through screening and risk factor identification critical for preserving vision. While the global prevalence of POAG in adults aged 40 and above is approximately 2.4%, African populations bear a disproportionate burden, with rates approaching 4.0% in sub-Saharan Africa [3].
The high prevalence of POAG in African populations has been attributed to a combination of genetic susceptibility, higher baseline intraocular pressure (IOP), and significant socioeconomic and healthcare access barriers. Established risk factors for POAG include advanced age, elevated IOP, African ancestry, male sex, family history of glaucoma, and thinner central corneal thickness (CCT) [4]. Recent meta-analyses have also highlighted associations with myopia and systemic comorbidities such as hypertension and diabetes [5]. In Tanzania, prevalence of 2-6. % among adults has been reported by various studies with elevated IOP and male sex emerging as dominant risk factors [6]. However, hospital- based data may overestimate prevalence due to the symptomatic nature of patients presenting at tertiary care facilities.
Genetic insights into POAG have expanded significantly over the past decade. Genome-wide association studies (GWAS) and post-hoc analyses of large trials, such as the Ocular Hypertension Treatment Study (OHTS), have identified multiple loci associated with POAG and demonstrated the utility of polygenic risk scores (PRS). Recent studied that looked at the OHTS found that individuals with high PRS had a 1.8-fold increased risk of developing POAG over 20 years, even after controlling for traditional clinical variables [5]. These findings suggest that integrating genetic profiling into routine risk assessment could enable earlier detection and individualized care, particularly in high-risk populations. However, such approaches are seldom applied in African healthcare settings due to limitations in infrastructure and accessibility to genetic testing and advanced diagnostics like optical coherence tomography (OCT).
In Tanzania and other low- and middle-income countries (LMICs), there remains a significant gap in implementing comprehensive POAG screening strategies that integrate ocular, systemic, and genetic risk factors. This study addresses this gap by synthesizing hospital-based data from the 2014 Muhimbili study with recent global literature from 2020 to 2025, aiming to contextualize POAG epidemiology and risk profiles in African populations. By aligning regional clinical evidence with international research advancements, the study advocates for the development of cost-effective, community-based screening programs. These should prioritize IOP measurement, systemic risk assessment, and, where feasible, genetic risk stratification, to reduce the burden of POAG-related blindness and promote equitable eye health across resource-constrained settings.
METHODOLOGY
Study Design
This study employed a dual approach, integrating a hospital-based cross-sectional study with a systematic literature review. The cross-sectional component was conducted at Muhimbili National Hospital (MNH) in Dar es Salaam, Tanzania, from June to December 2014, aiming to determine the prevalence and clinical characteristics of primary open-angle glaucoma (POAG). In parallel, a systematic review of global POAG literature published between 2020 and 2025 was undertaken to contextualize and update the hospital-based findings with contemporary evidence. The methodology adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [7].
Study Population and Setting
The hospital-based study included all new patients presenting to the outpatient ophthalmology unit at MNH during the six-month study period. MNH is the national referral and teaching hospital in Tanzania, receiving a wide spectrum of patients from across the country. A total of 876 new patients were screened, of whom 58 were diagnosed with POAG based on standardized clinical criteria and subsequently included in the analysis.
For the literature review, population-based and cohort studies were retrieved from PubMed, Embase, and Web of Science, focusing on both African and broader global populations. Inclusion criteria were: (i) cross-sectional or cohort design; (ii) use of the International Society of Geographical and Epidemiological Ophthalmology (ISGEO) or equivalent diagnostic criteria for POAG [5]; (iii) clear sampling methods; and (iv) extractable data on POAG prevalence and associated risk factors. Excluded were non-English publications, case series, studies without methodological transparency, and those focusing solely on secondary glaucoma.
Data Collection Procedures
For the hospital-based study, data collection was performed using standardized clinical assessment tools by trained ophthalmologists.
Evaluations included: Anterior segment examination via slit-lamp biomicroscopy, Visual acuity and refraction using autorefractors. Intraocular pressure (IOP) measurement with Goldmann applanation tonometry, Central corneal thickness (CCT) via ultrasound pachymetry, Visual field testing using the Humphrey Field Analyze Optic nerve evaluation with fundoscopy.
Socio-demographic data (age, sex), family history of glaucoma, and clinical findings were recorded using a structured, pretested questionnaire. POAG diagnosis was based on ISGEO guidelines [8], which require evidence of glaucomatous optic neuropathy with corresponding visual field loss and open anterior chamber angles confirmed by gonioscopy.
For the systematic review, two independent reviewers screened titles and abstracts, followed by full-text assessments. Data were extracted using a standardized form, including information on study design, sample size, population characteristics, diagnostic criteria, prevalence estimates, and identified risk factors (e.g., IOP, polygenic risk scores, hypertension). Discrepancies were resolved through consensus or third-party adjudication.
Data Analysis
For the hospital-based component, descriptive statistics were used to determine the prevalence of POAG, reported as a percentage with 95% confidence intervals. Socio-demographic and clinical variables were summarized using frequencies and proportions. Univariate logistic regression was initially performed to examine associations between individual risk factors and POAG. Subsequently, multivariate logistic regression identified independent predictors, reporting odds ratios (OR) with 95% confidence intervals. A p-value <0.05 was considered statistically significant. Statistical analyses were performed using SPSS version 25 (IBM Corp., Armonk, NY).
For the systematic review, a narrative synthesis was conducted to integrate findings on POAG prevalence and risk factors. Where applicable, meta-analytic estimates (e.g., pooled ORs, hazard ratios) were extracted. Emphasis was placed on findings from African populations. Notably, a 2024 post-hoc analysis of the Ocular Hypertension Treatment Study (OHTS) was referenced for insights on genetic risk, particularly polygenic risk scores (PRS) [9]. Comparative analysis was used to integrate hospital-based findings with contemporary global data to identify convergences and emerging trends.
Quality Control Measures
To ensure rigor in the hospital-based study, all clinical staff received protocol training. Instruments were calibrated regularly, and all assessments followed standardized procedures. Double data entry was implemented to minimize input errors, and cases with missing key variables (<5%) were excluded using listwise deletion.
For the literature review, methodological quality of included studies was assessed using the Newcastle-Ottawa Scale (NOS) [10], evaluating three domains: selection, comparability, and outcome. Only studies scoring ≥6 on the NOS were included. Quality assurance in data extraction involved dual review and consensus resolution
Ethical Considerations
The 2014 study received ethical approval from the Muhimbili National Hospital Institutional Review Board. Written informed consent was obtained from all participants after providing clear information about the study objectives, procedures, benefits, and risks. Participation was voluntary, and confidentiality was strictly maintained. The literature review did not involve primary data collection and thus did not require additional ethical clearance but followed ethical standards for secondary data use and transparent reporting, in line with the PRISMA 2020 update.
RESULTS
Prevalence of POAG
In the 2014 study, 876 new patients were screened at the Muhimbili National Hospital eye unit from June to December 2014, with 58 diagnosed with POAG, yielding a prevalence of 6.6% (95% CI: 5.0-8.5%). A 2021 meta-analysis of 50 population-based studies (198,259subjects) reported a lower African prevalence of 4.0% (95% CI: 2.0-2.8%) among adults aged 40+ years, with a global estimate of 68.56 million POAG cases in 2020 [11].
Socio-Demographic Characteristics
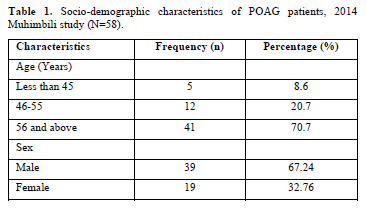
Table 1 summarizes the socio-demographic profile of the 58 POAG patients from the 2014study. The majority were aged 56 years and above (70.7%), with a male predominance (67.24%) and a male-to-female ratio of 2:1. The literature review confirmed higher POAG prevalence in men (OR 1.36, 95% CI: 1.23-1.52) and increasing prevalence with age, particularly in African populations (5.2% at 60 years, 12.2% at 80 years) [12].
Clinical Characteristics
All 58 POAG cases in the 2014 study were bilateral, with 55.17% reporting a family history of glaucoma (Table 2). Anterior segment examinations showed normal findings for conjunctiva, cornea, anterior chamber, and pupil in all patients, but 32.76% had premature cataracts. Refraction revealed myopia in 68.96%, with 79.31% having CCT<540 μm and all exhibiting visual field defects. Intraocular pressure (IOP) was 21-26mmHg in 82.75%, and 82.76% had a cup-to-disc ratio (CDR) >0.5. Nasal vessel shifting was present in 89.65%, and optic disc hemorrhage was rare (3.44%).

Risk Factors
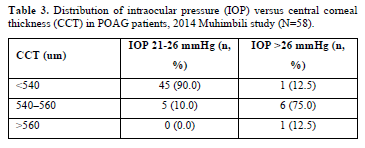
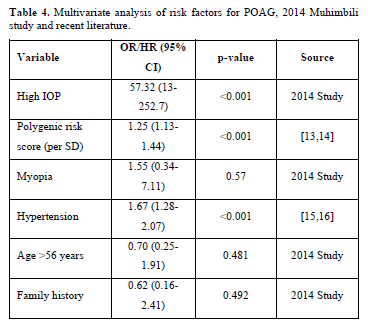
Multivariate analysis from the 2014 study identified high IOP as the strongest risk factor for POAG (OR 57.32, 95% CI: 13-252.7, p<0.001), with a significant association between IOP and CDR (p=0.001). Table 3 illustrates the distribution of IOP versus CCT, showing that 90% of patients with IOP 21-26 mmHg had CCT <540 μm. Recent literature reinforced IOP as the primary modifiable risk factor, with additional factors including myopia (155% higher incidence), hypertension (pooled OR 1.67, 95% CI: 1.28-2.07), and thinner CCT [13,14].
A 2024 OHTS post-hoc analysis (1009 participants) demonstrated that high polygenic risk scores (PRS) increased POAG risk 1.8-fold over 20 years (HR 1.25 per SD, 95% CI:1.13-1.44) [15]. Table 4 summarizes multivariate risk factors from both the 2014 study and recent literature, highlighting the prominence of IOP and genetic predisposition.
Synthesis with Recent Literature
The 2014 study’s findings align with recent literature regarding high IOP, male pre-dominance, and age-related risk, but the hospital-based prevalence (6.6%) exceeds the population-based African estimate (4.0%) [1]. Advances in genetic profiling (PRS) and recognition of systemic risk factors (e.g., hypertension) enhance risk stratification beyond.
DISCUSSION
The elevated burden of primary open-angle glaucoma (POAG) in African populations, as observed in the 2014 Muhimbili National Hospital study and corroborated by recent global meta-analyses, underscores a critical public health challenge. The higher prevalence reported a decade ago, with only slight changes over the past ten years, indicates that much work remains to be done to improve the condition. Additionally, clinical settings may introduce selection bias inherent in hospital-based studies, where patients often present with advanced disease. This discrepancy suggests that a substantial number of undiagnosed cases may exist within the community, particularly in regions with limited access to ophthalmic care. The consistent association of POAG with older age and male gender across studies points to demographic vulnerabilities that warrant targeted screening strategies [17]. This epidemiological pattern reflects both genetic predisposition and environmental stressors, necessitating a nuanced understanding of POAGs multifactorial etiology in African contexts. Advancements in diagnostic technology, notably optical coherence tomography (OCT)and polygenic risk scores (PRS), have revolutionized POAG risk assessment, offering precision that was unavailable during the 2014 study (18). OCTs ability to detect early retinal nerve fiber layer thinning contrasts sharply with the reliance on tonometry and visual field testing in resource-constrained settings like Tanzania. Similarly, PRS introduces a genetic dimension to risk stratification, identifying individuals at higher risk even before clinical signs emerge. integrating these tools could shift POAG management from reactive to proactive, but their inaccessibility in low-resource settings exacerbates health inequities. This technological divide challenges the global ophthalmology community to innovate affordable diagnostic solutions tailored to African health care systems.
The interplay of systemic risk factors, such as hypertension and myopia, with traditional ocular markers like intraocular pressure (IOP) and central corneal thickness, reveals POAGs complexity [19]. Systemic conditions may exacerbate glaucomatous progression through vascular dysregulation, a hypothesis supported by recent studies linking blood pressure extremes to optic nerve damage [20]. This insight shifts the paradigm from an exclusively ocular focus to a holistic approach, where cardiometabolic health is integral to POAG prevention. In African populations, where hypertension prevalence is rising, this connection demands interdisciplinary collaboration between ophthalmologists and primary care providers to address shared risk factors, potentially reducing POAGs burden through integrated health interventions. Socioeconomic barriers, including limited healthcare access and low awareness, amplify POAGs impact in settings like Tanzania. The 2014 study’s hospital-based design implicitly excluded rural populations, who face greater obstacles to care. community-based screening programs, leveraging mobile clinics and trained non-specialist health workers, could bridge this gap. Such initiatives, paired with public health campaigns to raise awareness, could enhance early detection, particularly among high-risk groups identified by family history or genetic predisposition [21]. The success of these strategies’ hinges on government and international support to fund infrastructure and training, ensuring sustainability in resource-limited environments.
Looking forward, a dual approach: scaling up affordable diagnostics (e.g., portable tonometers) and advocating for research into cost-effective PRS implementation is commendable. Future studies should prioritize longitudinal designs to track POAG progression in African cohorts, incorporating OCT and systemic risk factors to refine predictive models. Public health policies should integrate POAG screening into existing primary care frameworks, emphasizing hypertension management and genetic counseling where feasible. These efforts, grounded in the synthesis of historical and contemporary data, could transform POAG management, reducing preventable blindness and advancing health equity in African populations. The global ophthalmology community must act decisively to translate these insights into actionable change.
CONCLUSION
This study, integrating the hospital setting findings a decade ago with recent global research, underscores the persistent burden of primary open-angle glaucoma (POAG) in African populations and the urgent need for enhanced screening and management strategies. The synthesis reveals that while traditional ocular risk factors remain central, advancements in genetic profiling and recognition of systemic contributors offer new avenues for early detection. These insights highlight the importance of a multifactorial approach to POAG, particularly in resource-constrained settings where diagnostic access is limited. By bridging historical clinical data with contemporary evidence, this work emphasizes the potential for targeted interventions to reduce POAG-related blindness. The findings advocate for integrating affordable diagnostics, such as tonometry, into community-based screening programs to reach underserved populations in Tanzania and similar contexts. Future research should prioritize longitudinal studies incorporating advanced tools like optical coherence tomography and polygenic risk scores to refine risk stratification. Public health policies must embed POAG screening within primary care frameworks, addressing systemic risk factors like hypertension to maximize impact. Collaborative efforts between governments, international organizations, and researchers are essential to build sustainable ophthalmic infrastructure, ensuring equitable access to care and ultimately mitigating the global burden of POAG.
No Files Found
Share Your Publication :